Insurers cut back GLP-1 coverage as demand soars: Found study

As demand surges for GLP-1 therapies, insurers are pulling back on coverage, according to new data from obesity care provider Found. | Sarah Jones Simmer, CEO of Found, said that the trends are likely the result of irresponsible prescribing for recreational reasons causing the pendulum to swing "all the way in the other direction," and it's leading to patients who have genuine medical need struggling to access these therapies.
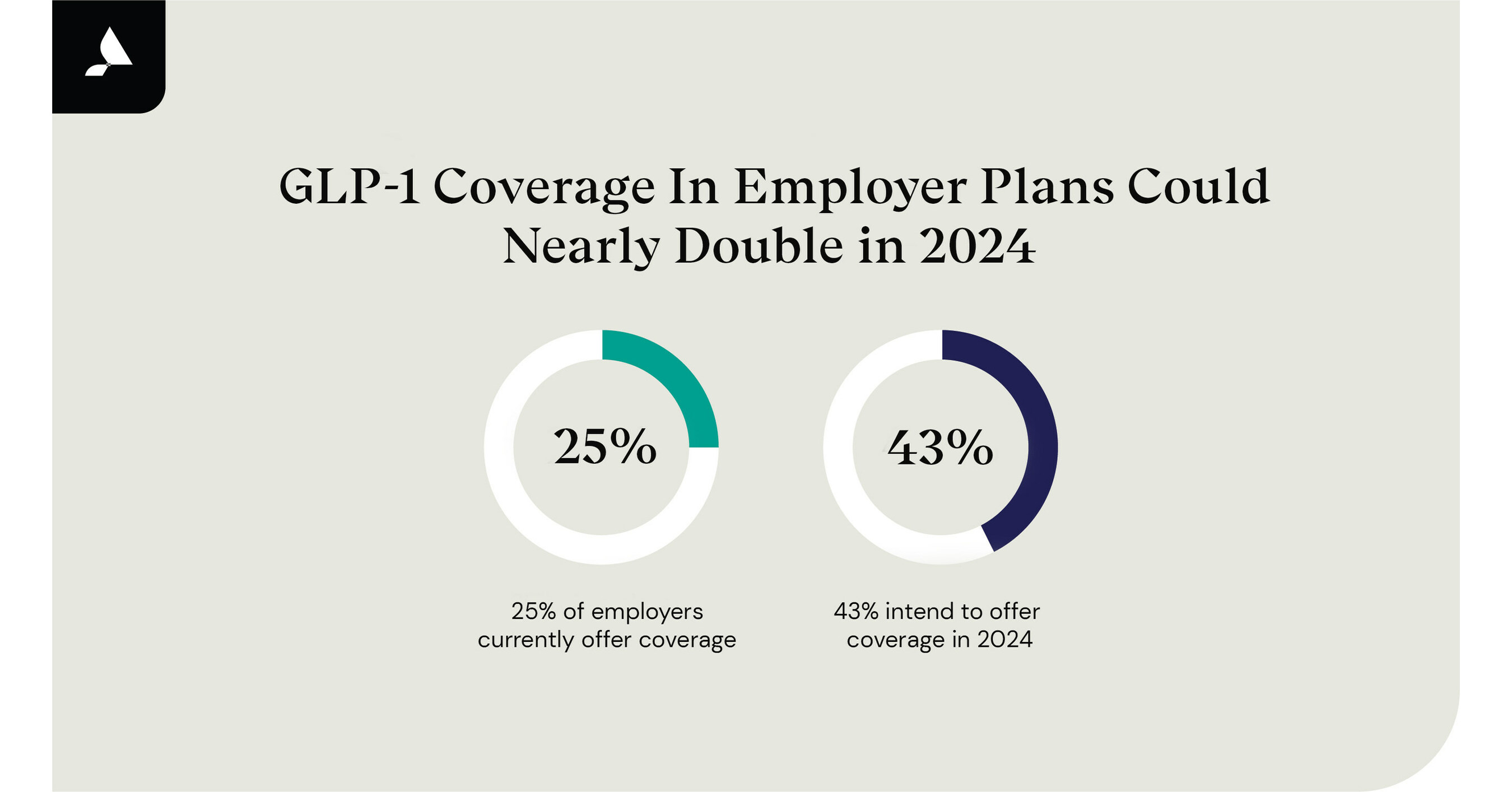
GLP-1 Coverage in Employer Plans Could Nearly Double in 2024
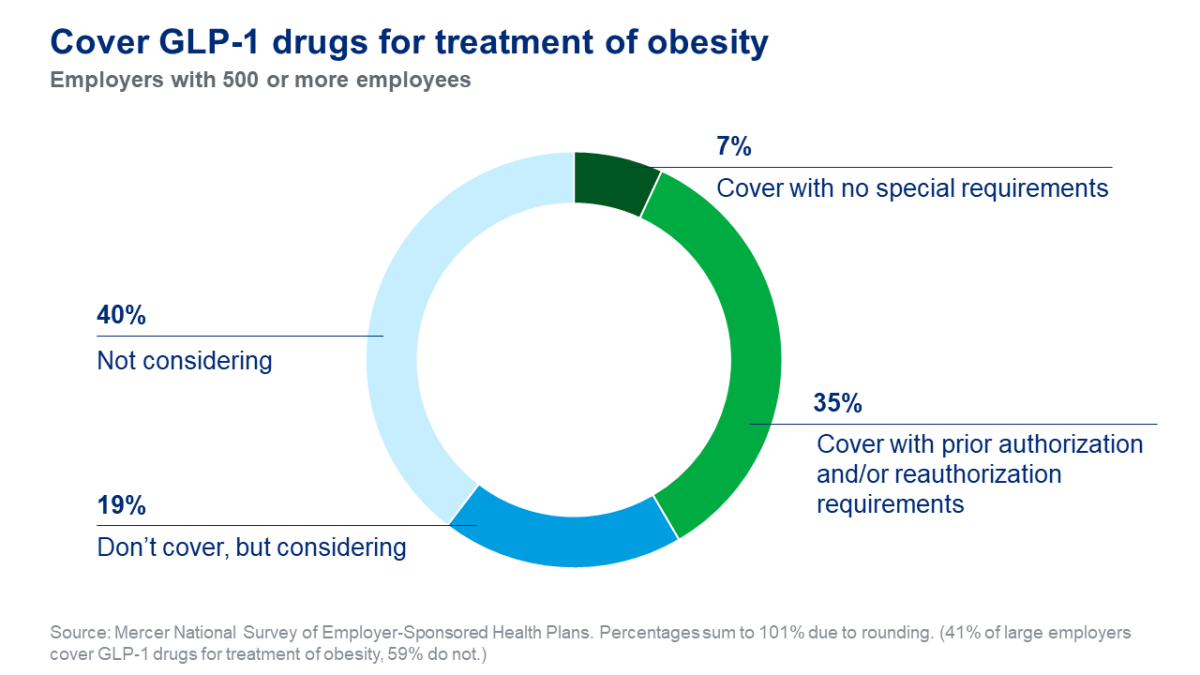
Designing fiscally viable coverage of GLP-1 weight-loss drugs
Denmark's largest health insurer drops weight-loss drug coverage
20% of Americans Would Change Jobs to Gain Ozempic, Wegovy Coverage

GLP-1 Receptor Agonist Shortage: Challenges and Solutions in Type

Jefferies highlights implications of weight loss drug GLP-1 on re/insurance sector - Reinsurance News

Focus: US diabetes patients face delays as insurers tighten Ozempic

Designing fiscally viable coverage of GLP-1 weight-loss drugs

Tsunami of exclusion': Patients face aftermath of GLP-1 cuts

U.S. employers covering weight-loss drugs could nearly double in 2024 - survey

106-Care of People with Diabetes - A Manual of Nursing Practice, 3 Edition-Trisha Dunning-1405170
Why Won't Your Company Pay for Weight-Loss Drugs Like Wegovy

GLP-1 Receptor Agonist Market Size, Share & Analysis, 2023-2032

U.S. employers covering weight-loss drugs could nearly double in 2024 - survey

The Rise of GLP-1 Receptor Agonists and Coverage Challenges